The FDA has approved Casgevy (exa-cel) for treatment of people ages 12 and older with sickle cell disease. Casgevy is the first therapy approved for use in the United States that uses CRISPR gene-editing technology to alter a patient’s genes.
“It’s tremendously exciting,” says hematologist-oncologist Monica Bhatia, MD, associate professor of pediatrics at Columbia University Vagelos College of Physicians and Surgeons, who has treated adolescents and teenagers with the therapy in the clinical trials that led to FDA approval. “By editing certain cells, we minimize symptoms, decrease pain, and decrease hospitalizations for people with sickle cell disease.”
Monica Bhatia (Photo credit: Columbia University Irving Medical Center)
Bhatia, who is chief of pediatric stem cell transplantation at NewYork-Presbyterian/Columbia University Irving Medical Center, led the Columbia team that treated pediatric sickle cell patients with Casgevy during the multi-center clinical trials. (Markus Mapara, MD, professor of medicine at Columbia and director of adult blood and marrow transplantation at NewYork-Presbyterian/Columbia University Irving Medical Center, led the team that treated adults with sickle cell disease in the same trial.)
Until now, the only long-lasting treatment available for sickle cell disease was a bone marrow transplant that gives patients a source of healthy blood cells from a donor. Outcomes are best for those who have matched sibling donors (who have similar immune system genes), but that applies to only 15% of people with this disease.
“After bone marrow transplants, our patients finish college, go on to jobs, bear children, have a family, have a life,” says Bhatia. “The sky’s the limit. Though one issue with transplants is that patients must take at least one immunosuppressive drug post-transplant and there’s always a risk that the donated cells will be rejected or even attack the patient’s organs.”
“With gene therapy, you don’t have to rely on a donor or worry that your body will reject the donated marrow or that the donated marrow will launch an attack. You rely on yourself,” says Bhatia. “You are the cure.”
FDA Approves Another Gene Therapy for Sickle Cell DiseaseAnother gene therapy for sickle cell disease, Lyfgenia, was also approved by the FDA on Dec. 8. With Lyfgenia treatment, a patient’s blood-forming stem cells are extracted and a harmless virus is used to insert a new hemoglobin gene into the stem cells before they are returned to the patient. The new gene stabilizes red blood cells and prevents them from becoming misshapen. NewYork-Presbyterian/Columbia enrolled adult patients in the trial that led to FDA approval of Lyfgenia.
We asked Bhatia to explain what sickle cell disease is and how Casgevy works.
What is sickle cell disease?
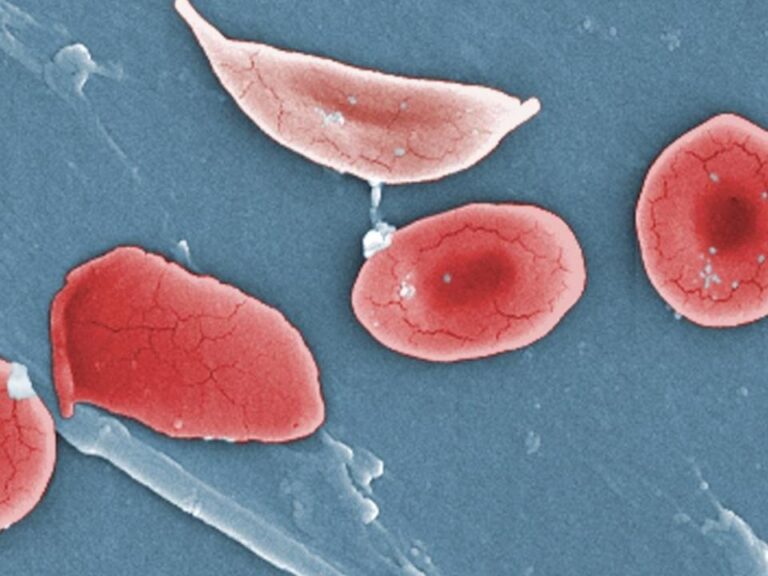
Sickle cell disease is a red blood cell disorder that affects about 100,000 people in the United States. Although sickle cell disease can affect anyone, it is most common in people of African descent and occurs in one out of every 365 Black or African American babies born each year in the U.S.
People with sickle cell disease inherit a gene from both parents that has instructions for making abnormal hemoglobin. The abnormal hemoglobin causes red blood cells to stiffen and become misshapen, changing from round to sickle-shaped. These cells do not flow easily through blood vessels, starving vital organs of oxygen, causing organ damage, strokes, and acute episodes of tremendous pain.
Sickle cell is a debilitating disease and people living with it have a shorter life expectancy.
What does it feel like to have sickle cell disease?
Everybody’s different. Many people need frequent blood transfusions and hospital care. Some live with chronic pain: There’s not a day in the lives of these patients when they don’t have some degree of pain, including regular bouts of extreme pain, called pain crises.
Some people have pain so distressing they go to the emergency room because medication and infusions are not enough to get relief. They miss work or school and it’s a challenge to hold steady jobs or meet academic expectations. Children are regularly left back in school.
Children as young as 8 are vocal about not wanting to be different. They want to play sports, go swimming, play with their friends. They wonder: Why am I the one in pain? Why are my eyes yellow? Things that may seem trivial, like when you can’t run as fast as everyone else in gym class, are actually significant and lead to distress on top of physical pain.
How does the new gene therapy for sickle cell disease work?
Casgevy edits a gene inside stem cells that controls the production of fetal hemoglobin, a type of hemoglobin we all produce until shortly after birth. Using CRISPR, a precise edit is made inside this gene, allowing stem cells to restart the production of fetal hemoglobin. When the red blood cells produce a certain level of fetal hemoglobin, the cells don’t become sickled or sticky. It’s a beautiful concept where you are reprogramming the patient’s own genes.
What’s involved in getting the new gene therapy?
With Casgevy treatment, the first step is removing some of the existing stem cells so that they can be edited in the laboratory with CRISPR before they’re returned to the patient.
Before the transplant, patients must be treated with chemotherapy in the hospital to make space in the bone marrow for the new blood-forming cells. The chemotherapy is very intense. It can have side effects including painful mouth sores, nausea, vomiting, diarrhea, hair loss, and long-term effects on fertility. The chemotherapy part of the treatment requires a lengthy, weeks-long hospital stay while the patient’s immune system recovers.
CRISPR ExplainedCRISPR is a gene-editing tool that can make precise changes to the DNA of living organisms. Read more about the potential of CRISPR to impact society in this interview with Columbia CRISPR expert Samuel Sternberg.
After the CRISPR-edited stem cells are transplanted, they start making red blood cells that contain fetal hemoglobin and the patient’s sickle cell symptoms subside or disappear as levels of fetal hemoglobin increase.
The result is that people who suffered daily and expected their lives to end in their 40s have a better quality of life and the hope that they will live into their 80s like everyone else. It gets me so excited every time I think about it!
But let’s acknowledge that with both a bone marrow transplant using donated cells and gene therapy you must first have chemotherapy to wipe out the bone marrow. I’ve had people come to me for a bone marrow transplant, and when they hear how intense chemotherapy is, they say, “You know what, I can’t do it. I’m going to wait for gene therapy.” But chemo is not something you can avoid with either therapy.
Can the new therapy be considered a cure?
We’re not sure yet. In the study, people who were treated with CRISPR gene therapy have been pain-free. Their lives are completely changed for the better. We hope things will stay that way.
Because the treatment is so new, however, we must wait to see if the results last. We’ll need to continue to follow these patients to see if the complications of sickle cell disease—organ damage and strokes, in particular—are prevented by the treatment. We’re participating in a trial that will follow the patients for the next 15 years to learn more.
How do we know the new therapy is safe?
The clinical trial tested the safety and efficacy of using CRISPR to edit the hemoglobin-producing stem cells in 31 patients with severe sickle cell disease as well as in 44 patients with another genetic blood disorder, beta thalassemia. With a gene editing approach there are concerns about unintended (off-target) effects. This continues to be studied and thus far, there have been no reports of this complication.
We and our trial colleagues have seen that the complications that arise are mainly due to the chemotherapy required during the transplantation process, not the gene therapy.
It’s important to get the treatment from a center that has a multidisciplinary team that is well-versed in the nuances of stem cell transplantation for sickle cell and is able to provide cutting-edge therapies to address infections and other post-transplant complications.
Will everyone with sickle cell disease be eligible for the new treatment?
The trial was only open to people who have had multiple pain crises, never had a stroke, and do not have a matched sibling donor for a bone marrow transplant, but we are hopeful that all people with sickle cell disease will have access to the treatment.
The trial also dovetailed with our mission to improve health equity outcomes for all people, including those from marginalized communities who are living with long-neglected diseases like sickle cell.
It’s an exciting time for sickle cell disease treatments overall. For many years, hydroxyurea, a medication that reduces pain crises and the need for blood transfusions, was the only drug therapy available. In the last five years, numerous new disease-modifying drugs have been approved to reduce the symptoms of sickle cell disease, and more gene therapies are being tested in clinical trials, showing good results so far. Plus, outcomes for bone marrow transplantation are better than ever. I’m really hopeful about the future of sickle cell treatment.